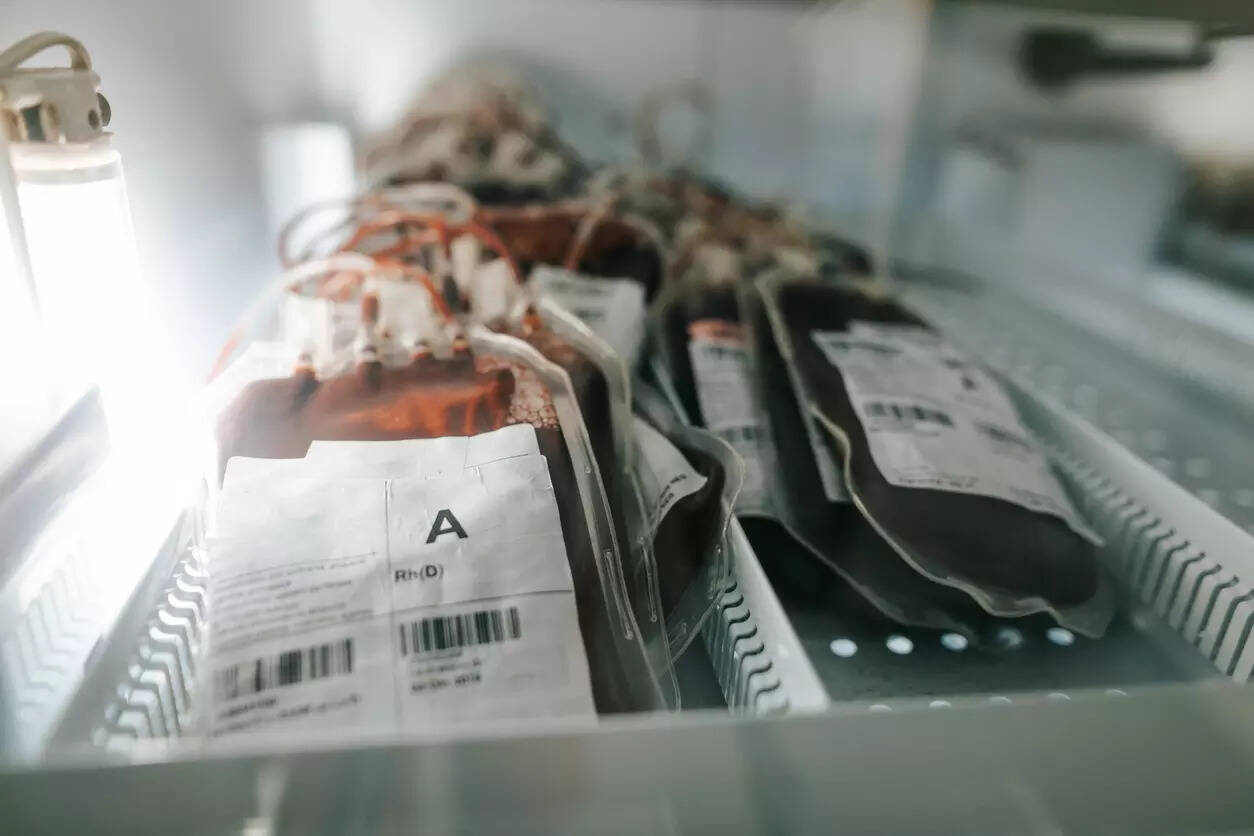
New Delhi: Diagnosed with thalassemia at the age of two, a 23-year-old woman depended on blood transfusions every three weeks to stay alive.
But when she was hospitalised with dengue in Class VIII, doctors discovered something more alarming – she was diagnosed as HIV-positive. “I wasn’t recovering. After several tests, they told me I was HIV-positive. I suspect it came from a transfusion. If the blood was properly tested, maybe this wouldn’t have happened,” she said.
Now living with both thalassemia and HIV, she depends not only on regular transfusions, but also on antiretroviral treatment.
The woman’s testimony at the roundtable on “Ensuring Safe Blood for All: Strengthening Blood Safety Practices”, organised by the Thalassemia Patients Advocacy Group (TPAG) at India International Centre on Thursday, brought into sharp focus the urgent need to fix India’s entire blood safety ecosystem.
Experts at the event called for comprehensive reforms – from mandatory nucleic acid testing (NAT) at all blood banks to boosting voluntary blood donation and patient participation in policymaking. NAT, which detects HIV, Hepatitis B and Hepatitis C during the early infection “window period”, is far more effective than standard tests, but is not yet mandatory across India.
“Safe blood is not just about testing – it begins at the source,” said Dr Sangeeta Pathak, secretary general of Indian Society of Blood Transfusion & Immunohematology (ISBTI) and head of Transfusion Medicine at Max Saket.
“Voluntary, non-remunerated blood donation is key. Sri Lanka has achieved 100% voluntary donation. Why not India?”
She called on both professionals and the public to take ownership. “We must talk about it, promote it, and strengthen the culture of safe, voluntary blood donation.”
Anubha Taneja Mukherjee, member secretary, TPAG, reminded participants that blood safety is a matter of human rights. “This isn’t just a technical issue. It’s about dignity, equity, and the right to safe, life-saving interventions.”
Public health advocate Prof Bejon Kumar Misra emphasised the need for transparency and accountability. “Safety is non-negotiable. People have a right to know what is being done – and what’s not. Communication is critical. We need strategies that ensure no patient falls through the cracks.”
P C Sen, senior Supreme Court advocate, reiterated the state’s legal obligation to ensure access to pathogen-free blood.